Drawing Attention to Public Health
Remembering the Spring

Photo by inma · lesielle on Unsplash
Writing for MyUVic Life has been a privilege.
Since the first stay home order, my posts were able to continue, despite restrictions in all other areas of my life.
Being a student of public health, I have been fortunate to explore topics of popular interest because the public is so acutely aware of health during this pandemic.
On April 6th I wrote a blog post about risk factors for disease and how we have an opportunity through this health crisis to explore ways to improve the health of the population as a whole.
In that post I reflected: “As I contemplate this current crisis, I can appreciate how those of our society who are most vulnerable are the ones that will have the hardest time coping with these health directives we have all been given.” This statement is true even as new public health ordes have been given in BC and around the country to once again restrict social activities.
Defining What is Essential

Photo by Aaron Burden on Unsplash
My next post published on April 15th looked at the question of essential services for health and how we define what is essential to whom. When we lose our social life, many informal supports break down, making it harder to follow health directives.
“The average person that is already struggling with social isolation is going to have a difficult time without being able to get out and gather.”
Many people have already experienced the hardship of social isolation during stay home orders, business closures, and community social services, or supports like drop-in groups and public gathering spaces.
Does this news stress anybody else? It’s enough to weaken my immune system! Self-isolation is compounded by constant and repeated news blasts stating case counts and reporting on the spread of coronaviruses detected in public health laboratories.
I also wrote about the impact of stress, and how it relates to our resistance to infection and disease.
I explored that topic in a post published on April 24th. “People living ‘in survival’ – paycheque to paycheque, in precarious work, with unsafe or unhealthy housing, in abusive relationships, and in inner-city neighbourhoods,” are at greater risk to COVID-19 and other respiratory infections, as there is health disparity within our populations (see Davidson, 2015).
Silent Hypoxia

Photo by Fabien Maurin on Unsplash
Then in May, some good news. I watched an interview on PBS with Dr. Richard Levitan, an airway specialist working in NY, talking about how doctors are getting better at treating infections and pneumonia from the coronavirus, creating better outcomes.
He also published an opinion paper in the New York Times which is wonderfully informative, called The Infection That’s Silently Killing Coronavirus Patients: This is what I learned during 10 days of treating Covid pneumonia at Bellevue Hospital. They were learning to treat infection better, prevent death, and I was starting feeling some hope.
Now we have a name for it – Silent Hypoxia.
Silent hypoxia describes how people developing advanced pneumonia from a novel coronavirus infection do not present the usual symptoms of low oxygen, or pass out suddenly, until advanced stages of pneumonia have already set in.
“People are in the waiting room on their cellphones” says Dr. Levitan, and their lungs are worse than you would ever imagine, with oxygen levels so low that it is a wonder they are even conscious.
The lesson there is to test all symptomatic people for coronavirus and monitor oxygen early on in the disease pathology to prevent having to use ventilators in late stages of this disease.
The Many Consequences of Lock Down

Photo by thr3 eyes on Unsplash
We told people to stay home if they have symptoms, but for some that is painfully difficult, and perhaps bad for their health.
This led me to explore the balance between the acute care setting that supports patients to recover, and other determinants of health.
In this post I present the social determinants of health and how, as a society, we can be better protected from disease with improved social conditions, especially for those who are living in poverty, or are already isolated.
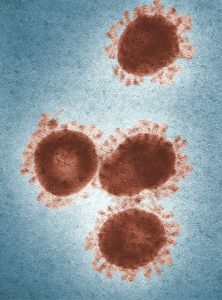
Photo by CDC on Unsplash
If we consider how existing social problems, like housing and food insecurity, play on a health crisis such as we are facing, we can see how the closure of a food bank, or shutting down meal programs will impact the people who are already experiencing great hardship.
One food bank I am familiar with could not find the volunteers who would come to work during the lock-down. Their hours were also reduced, despite increased demand for foods.
As we enter into this new time of restriction, let’s learn the lessons from our first encounter with the novel coronavirus.
I think we need to take a good hard look at how we manage health preventatively even while we contain this current crisis.
Stay safe.
Aaron
Ref: Davidson, A. (2014). Social determinants of health: A comparative approach. Chicago.




Well done Aaron !!! Love you
Aaron, Appreciate the journey of this article. Well Done!
Thank you both!