A knowledge synthesis
By Cara Pearson, Pat Porterfield, Rick Sawatzky & Kelli Stajduhar
Beginning in 2011, a team of British Columbia nursing researchers, practitioners and administrators, known as Initiative for a Palliative Approach in Nursing: Evidence and Leadership (iPANEL, ipanel.ca), came together. Much of what is known about caring for people who are approaching end of life comes from our experiences of caring for cancer patients. We recognized that people who were dying from chronic, life-limiting illnesses, such as dementia, frailty, COPD and kidney disease, do not receive adequate palliative care services. We also recognized that most people with these long-term advancing illnesses could be better served by a different type of care. A palliative approach to care has become increasingly taken up in other parts of the world. iPANEL was formed with the goal of furthering the integration of a palliative approach throughout the BC health care system in order to improve care for those with chronic life-limiting illness and their family members.
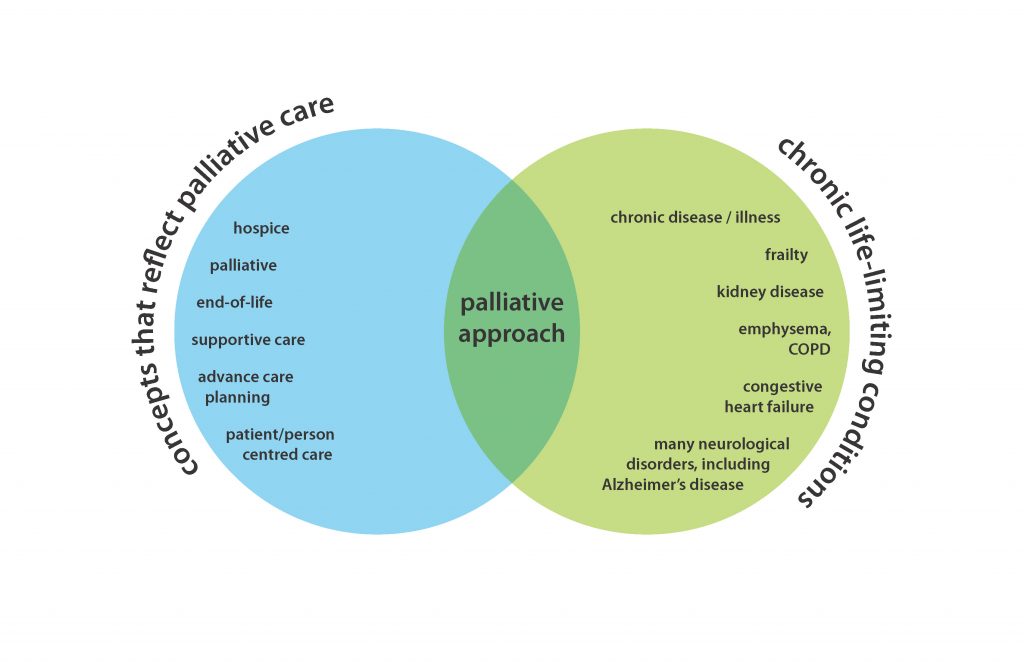
One of the first of many projects undertaken by members of the iPANEL team was a knowledge synthesis on how a palliative approach is delineated in the literature. This knowledge synthesis has now been published and is available open access: Conceptual foundations of a palliative approach: A knowledge synthesis (http://www.biomedcentral.com/1472-684X/15/5). The goal of this research was to clarify the meaning of a “palliative approach” to care for people who have chronic life-limiting conditions. We began with the knowledge that in order to care for this particular patient population, this required a blending of palliative care and chronic disease management principles and practices. A comprehensive search of 11 research databases for the intersection of these terms (see diagram) generated 190,204 search results. In order to sift through this many documents, a probabilistic, iterative computer-assisted screening program was developed and utilized alongside manual screening (see the full article for more detail), resulting in a final set of 91 research articles included for analysis. Narrative synthesis and thematic analysis methods were applied to conceptualize key characteristics of a palliative approach.
This research shows that there is a distinction between a palliative approach and the way palliative care has been enacted as a specialized service. Three key features of a palliative approach include: (1) upstream orientation towards the needs of people who have life-limiting conditions and their families, (2) adaptation of palliative care knowledge and expertise, and (3) operationalization of a palliative approach through integration into systems and models of care that do not specialize in palliative care.
(1) Upstream orientation to care
A palliative approach to care begins by recognizing the life-limiting nature of many chronic conditions. Applying palliative care principles earlier in the course of an illness requires having an understanding of different chronic disease trajectories in order to determine where a person is on that trajectory. With this understanding, the changing needs of patients and families can be better identified and addressed, for example through proactive care planning, informed decision making, and advance care planning.
(2) Adaptation of palliative care knowledge and expertise
A palliative approach goes beyond simply applying knowledge and expertise from palliative care to practice; it requires adaptation to different patient populations and their unique disease profiles, in particular, accommodating the uncertainty inherent in many disease trajectories. Adaptation of symptom management, communication with patients and families, and partnership strategies were evident in the literature.
(3) Integration and contextualization within the health care system
Delivering a palliative approach early in illness trajectories necessitates greater capacity within the health care system to recognize and to address the evolving care needs of people with chronic life-limiting conditions. There is no single model of care delivery that best enables a palliative approach to care. Rather, a palliative approach integrated and embedded throughout all existing providers and settings of the health care system is most likely to have a meaningful impact. Three prominent models for integration emerged: (1) into
generalist practice, (2) into disease-specific approaches, and (3) early in the disease trajectory.
Model 1: Integration of a palliative approach into generalist practice
The key feature of this model is the integration into care sectors rather than into specific disease care plans, enabling flexibility when caring for people with multiple co-morbidities. One example is the Gold Standards Framework (GSF) in the United Kingdom, which focuses on primary and residential care settings, and advocates for a total system transformation to care of the dying. The GSF provides education and capacity-building for all members of the care team. Overall, this model involves palliative care specialists working with generalist care providers to build capacity for delivering a palliative approach.
Model 2: Disease-specific approaches to care delivery
The key feature of this model is that palliative care principles are adapted and integrated into all sectors of the health care system so that people who have particular life-limiting conditions are supported throughout their illness progression. This involves collaboration between palliative care and chronic disease or geriatrics care providers, and coordination across health care sectors to ensure a full breadth of services. One example of this is chronic care teams and community health nurses working collaboratively through information technology to support COPD patients and their families. This necessitates ongoing capacity building for a palliative approach through intentional partnerships.
Model 3: Applying palliative care “early” in the disease trajectory
The key feature of this model is that it closely resembles traditional palliative care but is delivered earlier than it traditionally would be, typically by palliative care specialists. One example is outpatient visits with specialist palliative care providers where patients who had been diagnosed with metastatic non-small-cell lung cancer were able to discuss symptoms, goals of care, decision-making and care coordination. This model relies on increased and routine involvement of palliative care specialists early in and throughout the illness trajectory, and has mostly been applied in populations of cancer patients. Given the focus on cancer, less adaptation of
palliative care knowledge is required.
The findings of our knowledge synthesis provide much needed conceptual clarity regarding a palliative approach. Such clarity is of fundamental importance for the development of healthcare systems that facilitate the integration of a palliative approach in the care of people who have chronic life-limiting conditions.
From the 2016 Spring Communiqué — Knowledge Synthesis
Recent Comments