Guidelines exist for one of the world’s most dangerous and widely used drugs, alcohol. These were developed to help people and health care professionals have some idea what different level of drinking might be associated with low, moderate and high risk of harm. They are based on evidence, and although recent epidemiological data has probably underplayed the risks for cancer, properly used (e.g. within brief screening and intervention), they can help people reduce their drinking.
The problem is similar sensible guidelines don’t exist for illicit drugs. In most countries, the government line is basically, “Do not take illegal drugs because they are all bad.”
Just for the record (and the lawyers) the Global Drug Survey (GDS) states categorically that the only way to avoid all harm from drug use is to not use them. However, it’s not a very practical goal for people who like to indulge. The reality is that the risks of experiencing harms from using drugs can actually be massively reduced for most people with the right set of advice.
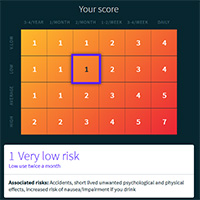
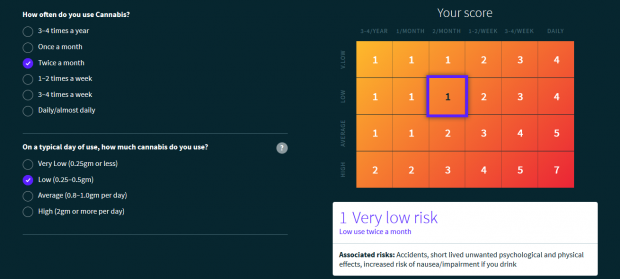
This is why GDS developed the world’s first Safer Using Limit guidelines. Using data collected from the 100,000 people who took part GDS2015, we are creating a number of guidelines, starting with cannabis, aimed at raising people’s awareness of the level of risk that different patterns of drug use places them at. We did this by asking respondents to rate how the risk of harm from different drugs (including alcohol) is heightened with increasing levels of use. “Risk” here refers to the probability, range and severity of harm. The higher the score, the more likely it is for a person to experience harms and problems, with higher scores indicating an increased severity of said harms. We also asked our respondents to think about the likelihood of a person experiencing harm over the next 1-2 years. By harm, we mean anything that causes a person problems, such as mental or physical health, relationships and behaviours, finances or ability to work, study, or just do the things in life they want to do.
Our first set of guidelines (on cannabis) was launch on June 18th 2015 at www.saferuselimits.co. Over 20,000 people have got their risk score so far.
Are drug users really the best experts?
A reasonable question to ask is, how valid are risk estimates based on the votes of a self-selecting group of drug users who surely have cognitive and emotional bias to minimize the risks associated with a consumptive behavior? I don’t know, but leave it to you to decide based the composite ratings from over 40,000 cannabis users that Professor Michael Linskey used to help develop the relative risk scores – shown below.
I came up with very similar ratings when I did the exercise blind before we launched GDS2015 last year. We hope to ask experts around the world to do the same thing in a project we are trying to set up to see the level of agreement between users and “experts.” The reality is, though, that the major driver for the approach we took was the fact that the people drug users trust most are other drugs users. Simply put, guidelines on safer-use limits voted by those who like to toke will be less quickly dismissed by other stoners.
I passionately believe that for most people who choose to use drugs and alcohol, they can be a source of pleasure that enhances the rich fabric of their lives. While I understand that drug use for some people is unwise (and best avoided) either because of their age, pre-existing health conditions or other vulnerabilities, the decision to use drugs is one that must always be treated with respect. I hope our work helps people, communities and governments have more honest conversations about drugs.
Author: Dr. Adam R Winstock MBBS, BSc, MSc, MRCP, MRCPsych, FAChAM, MD
Founder and Director, Global Drug Survey; Consultant Psychiatrist and Addiction Medicine Specialist, SLAM NHS Trust; Senior Lecturer, Kings College London
Twitter:
@globaldrugsurvy
@drugsmeter
(Author’s note: Want to help contribute to this research? We will be launching GDS2016 in November, 2015 with focuses on psychedelics, safer MDMA dosing, drug vaping and drug tourism. We are hoping to increase our Canadian participation this year, so don’t hesitate to contact me if you would like to help us spread the word.)
**Please note that the material presented here does not necessarily imply endorsement or agreement by individuals at the Centre for Addictions Research of BC